Individuals may experience seizures after head injury depending on the areas of the brain affected. For example, an injury to the frontal lobe can increase the risk of a frontal lobe seizure. Generally, the more severe a traumatic brain injury, the higher the chances of developing a seizure.
Understanding how a post traumatic seizure may occur can help you and your loved one take the necessary safety precautions. This article will discuss the potential causes of seizures after head injury, along with the various types and treatments.
Can a Traumatic Brain Injury Cause a Seizure?
In a simple answer, yes, a traumatic brain injury can cause a seizure. A seizure occurs when there is a sudden, disorganized or burst of electrical activity in the brain. When the electrical signals cross each other, it can cause the brain and body to short-circuit, resulting in a seizure (uncontrollable shaking or convulsion).
Studies show that individuals who have sustained severe traumatic brain injuries are at an increased risk of having a seizure. According to the CDC, roughly 10% of those who require hospitalization after a TBI experience a seizure.
There are various types of seizures that can occur depending on the severity and potential causes. Two of the main classifications are early post traumatic seizures, which occur within the first seven days after a head injury, and late post-traumatic seizures which occur after seven days.
Studies also show that about 80% of survivors who experience late post traumatic seizures will develop post-traumatic epilepsy. Epilepsy is a condition where individuals experience multiple (two or more) seizures.
Post-traumatic seizures can be provoked or unprovoked. Provoked seizures usually occur immediately after a head injury but may not be directly caused by damage from a TBI.
Researchers believe certain factors can increase the risk of developing a seizure after sustaining a head injury. Risk factors including intracranial hemorrhage (brain bleed), penetrating TBIs, loss/lack of sleep, antidepressants, and alcohol. Other factors such as a high-fever, severe infection, or kidney failure can also make TBI survivors more susceptible to seizures.
However, some individuals may experience a seizure without any of these risk factors, known as unprovoked seizures. Unprovoked seizures occur at least one week after a TBI and can arise directly from TBI damage or have unclear causes. Some of the most common unprovoked seizures occur within the first 24 hours after a head injury.
There are various types of seizures that can occur after a head injury depending on the severity and location of the injury. Let’s take a look at what they may be.
Types of Focal Seizures After Head Injury
Seizures can begin in one small part of the brain and last for a few seconds, or it can spread throughout the brain and occur for minutes.
More specifically, focal seizures (also known as partial seizures) start in one area of the brain and spread across the brain and cause mild or severe symptoms. Focal seizures vary depending on the areas of the brain damaged after a head injury. This includes:
Temporal Lobe Seizure
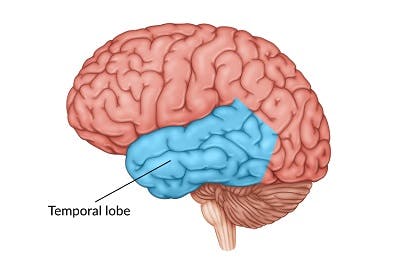
The temporal lobe is located beneath the temple of both sides of the head. The temporal lobe is mainly responsible for memory, emotions, interpreting sound, and understanding language. Damage to the temporal lobe can increase the risk of temporal lobe seizures, the most common type of epilepsy. Seizures in the temporal lobe vary in intensity, and some may be extremely mild that individuals barely notice them.
For instance, a survivor may get an odd feeling in the stomach or smell something “funny” or strange. Other times, an individual may be consumed by feelings of anxiety, fear, deja vu, or loss of reality. Survivors who experience temporal lobe seizures tend to perform repetitive movements (automatisms), which can include lip-smacking and rubbing both hands together.
Frontal Lobe Seizure
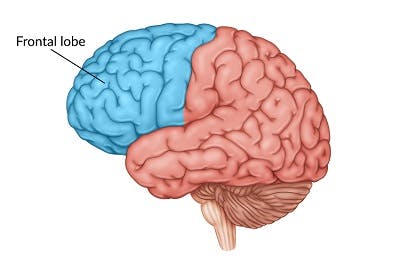
Frontal lobe seizures are the second most common type of epilepsy. They often occur at night while sleeping. The frontal lobe is located behind the forehead and is primarily responsible for movement, decision making, problem solving, as well as emotions. Depending on the damage to the frontal lobe, symptoms may consist of night waking, thrashing, and bicycling movements of upper and lower extremities.
Occipital Lobe Seizure
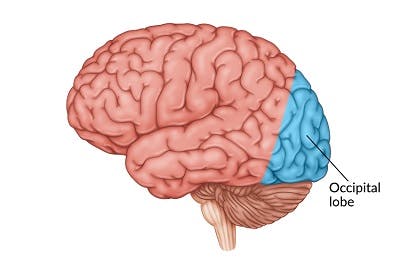
The occipital lobe sits at the back of the brain, behind the parietal and temporal lobes, and is responsible for visual perception including form, color, and motion. Occipital lobe seizures make up about 5% of all seizures in individuals with epilepsy. While the exact cause is unclear, individuals with damage to the occipital lobe such as a lesion are more likely to experience occipital lobe seizures.
Occipital lobe seizures can start with visual hallucinations of flickering or colored lights. Some symptoms may occur spontaneously or be triggered by visual stimuli such as a repetitive pattern or flashing lights. Often, occipital lobe seizures can be mistaken for migraine headaches because of the shared symptoms such as partial blindness, nausea, and vomiting. Speak with your doctor to obtain a proper diagnosis.
Parietal Lobe Seizure
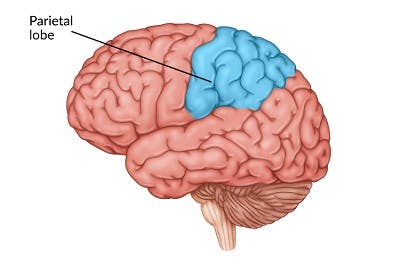
The parietal lobe is located near the center of the brain and is mostly responsible for processing information regarding touch, pain, and space. Similar to the occipital lobe, parietal lobe seizures comprise only about 5% of all focal seizures. Individuals who sustain a parietal lobe seizure often experience a disconnect between themselves and the somatic senses of the body.
Types of Generalized Seizures After Head Injury
Generalized seizures are the other types of seizures that can start as focal seizures and spread to both sides of the brain. They can also occur simultaneously over both sides of the brain, known as generalized onset. This includes:
Tonic-Clonic (Grand Mal Seizures)
Tonic-clonic seizures start on both sides of the brain, causing the body to stiffen (tonic phase) and then shake or convulse (clonic phase). These types of seizures are unique because they can develop from generalized seizures or focal seizures.
Absence (Petit Mal Seizures)
These seizures are brief and usually do not cause an individual to fall or have shaking movements. Absence seizures typically involve a sudden cessation of movement, along with staring and/or blinking. These seizures tend to last between 3 to 10 seconds, without confusion before or after. Absence seizures are also known as childhood absence epilepsy because of its common occurrence in early childhood. If it persists into adulthood, individuals may develop tonic-clonic seizures.
Myoclonic Seizures
Myoclonic seizures are sudden, jerking movements in a muscle or groups of muscles (arms, head, and neck), typically on both sides of the body at the same time. Myoclonic seizures commonly occur in the morning. While these seizures can begin in childhood, they can occur at any age. When myoclonic seizures are developed in adolescence with tonic-clonic seizures, they can lead to juvenile myoclonic epilepsy.
Tonic and Atonic Seizures (“Drop Attacks”)
Tonic and atonic seizures consist of sudden stiffness in the arms and legs, causing falls and injuries. These seizures are most common in individuals who sustained multiple TBIs, struggle with an intellectual disability, or have a condition known as the Lennox Gastaut Syndrome.
Individuals with a brain disorder may also experience atonic seizures, which consists of sudden loss of body tone that can result in collapsing or injury. A sequence of a tonic seizure followed by an atonic seizure are known as “drop attacks” and are often managed by medication, nerve stimulation, and/or diet therapy.
Both focal and generalized seizures have different underlying causes with a wide range of symptoms. Some types of seizures have warning signs that individuals may experience right before. Therefore, it helps to know what these signs are to help you and your loved one be more prepared in the case of a seizure after head injury.
“Seizure Aura” Symptoms: Know the Warning Signs of Post-Traumatic Seizure

An individual may notice minor symptoms, known as an aura, right before a seizure occurs. An aura refers to a different or unusual feeling, experience, or movement. For instance, survivors may have altered feelings, strange or “out of body” sensations, or sense of smell. These “seizure aura” symptoms may be physical or cognitive.
Signs of a seizure aura include:
- Blurry vision or partial vision loss
- Flickering or flashing lights
- Unusual smell
- Confusion
- Losing familiarity of people you know
- Feelings of panic or detachment
- Strong sudden emotions of joy, sadness, fear, or anger
- Sudden bitter, sweet, salty, acidic, or metallic taste
- Nausea
- Numbness or tingling sensations
- Buzzing or ringing in the ears
- Headache or lightheadedness
Unfortunately, only the individual themselves will notice or feel the signs of a seizure aura. If you experience any of these potential warning signs, get yourself into a safe position immediately and call for help. We will discuss what a safe position is next.
Usually, after the aura passes individuals can become unresponsive. Therefore, you may not be able to respond immediately if someone calls your name, or even blink if somebody waves a hand in your direction. For survivors, ask a loved one to stay close to your side. To caregivers, do your best to comfort the survivor and seek immediate help.
What to Do When Someone Has a Seizure After Head Injury

Knowing the signs and symptoms can help you and your loved one prepare and take the necessary precautions. Therefore, it’s crucial to know what to do and what not to do when someone is experiencing a post-traumatic seizure.
During the seizure, the electrical disturbance in the brain can cause several symptoms such as:
- Strange, jerky movements in the head, body, arms, legs, and eyes
- Staring
- Unresponsiveness
- Fumbling movements
- Lip-smacking
- Sudden tiredness and/or dizziness
- Inability to speak
- Trouble understanding others
Depending on the type of seizure, it can last for a few seconds or a couple of minutes. After it ends, individuals may feel weak, dazed, or confused. Fortunately, these effects eventually subside. To help ensure your loved one’s health and safety, it helps to know what to do in the event of a seizure.
Here are the do’s and don’ts of steps to take when someone is experiencing seizures after head injury:
DO:
- Loosen any tight clothing. Try to untie and loosen clothing, especially tight clothing around the neck area.
- Get the individual to the ground. Help the individual get to the ground and roll them to their side. This will help prevent choking and possible injury.
- Remove any sharp or hazardous objects away from the survivor. This will help reduce the risk of injury.
- Time the seizure. Grab a watch or timer to measure the length of the seizure. If a seizure lasts more than 3 minutes, call 911 immediately.
- Offer reassurance. After a seizure ends, the person may feel confused, anxious, and possibly embarrassed. It’s important to comfort them and let them know everything will be okay.
DO NOT:
- DO NOT hold the person down. Trying to hold them still will only hurt the individual more and may cause them to panic. Give them space while the seizure happens.
- DO NOT put anything in the person’s mouth. While an individual may bite their tongue or smack their teeth, do not attempt to put something in their mouth. This poses a major choking hazard. Do not attempt to give them water either until the seizure subsides.
- DO NOT encourage the survivor to drive, eat alone, or be near water without someone with them in case of another seizure.
Thus, it can also help to set up a Seizure Response Plan with your loved ones to be prepared in the case of a seizure after head injury. For individuals who have experienced a post-traumatic seizure, be sure to share this information with your friends and family so that they know how to assist you.
Treating Post-Traumatic Seizures
Treating seizures after head injury may vary depending on the cause and severity. It’s important to obtain a proper diagnosis from your doctor in order to receive appropriate treatment. An accurate diagnosis can also help identify the cause(s) of focal and generalized seizures.
Fortunately, there are several types of treatments your doctor may recommend. For many individuals, this includes prescribed anti-seizure medication that helps reduce seizure frequency and severity.
Some of the most common medications doctors may recommend for a post-traumatic seizure include:
- Clonazepam (Klonopin)
- Carbamazepine (Tegretol)
- Gabapentin (Neurontin)
- Phenytoin (Dilantin)
- Valproic acid (Depakene)
Every head injury is different as well as every seizure. Some post traumatic seizures can be more difficult to control and may require more invasive treatment when medication is not enough.
For example, some doctors may recommend trying Vagus Nerve Stimulation (VNS) Therapy. With VNS, a device known as the vagus nerve stimulator is implanted to help stimulate your nerves with electrical impulses. This proper flow of electrical impulses can help reduce and prevent future seizures.
Another method that can help treat post traumatic seizures is diet therapy. This is an approach used in conjunction with seizure medication to help control seizures. Two of the most popular diets are the Ketogenic Diet and modified Atkins Diet. Both should be monitored by your doctor and dietitian.
Additionally, survivors with a focal scar or other lesions in the brain may benefit from epilepsy surgery, however this is a highly invasive treatment. Be sure to speak with your doctor first to find the most suitable treatment for you.
Overcoming Seizures After Head Injury
Individuals may experience seizures after head injury depending on the severity and location of the injury, especially the frontal lobe. Seizures can be provoked by a number of risk factors or be unprovoked. Nonetheless, knowing the warning signs and symptoms of a post traumatic seizure can help you and your loved one take the necessary precautions and seek the proper help.
A post-traumatic seizure can occur just once or, when it occurs more than once, can be diagnosed as post-traumatic epilepsy. Fortunately, there are multiple ways to lower the risk of seizure after head injury. This can include prescribed medication, implant devices, and diet therapy.
We hope this article has helped you understand how seizures after head injury can occur and the steps to take to ensure your safety. Be sure to consult with your doctor for a proper diagnosis and the best possible treatment for a post traumatic seizure.
The post Seizures After Head Injury: Understanding How a Post-Traumatic Seizure Can Occur appeared first on Flint Rehab.



