Foot drop after TBI refers to the inability to lift the front portion of the foot, a movement known as dorsiflexion. This is caused by a disruption in the areas of the brain responsible for movement. When the brain cannot send the appropriate signals to lift your foot, foot drop may occur.
Individuals with foot drop have difficulty walking and safely navigating daily activities. Fortunately, there are various treatment options available to help improve foot drop after TBI.
This article will discuss the causes of foot drop after TBI, potential secondary effects, and therapist-recommended treatments.
Causes of Foot Drop After TBI
Lifting the foot up towards the shin is referred to as dorsiflexion. When the brain sustains an injury, the nerves responsible for activating the muscles in the front of the shin can become damaged. Without the appropriate nerve signals, the brain is unable to tell the muscles in the foot when to contract or relax, resulting in foot drop.
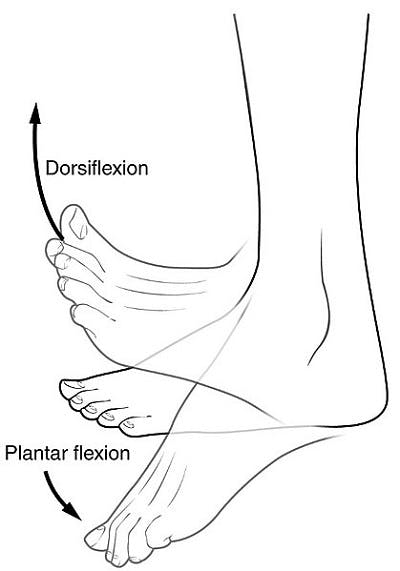
Image Credit: Wikipedia
Fortunately, the brain has the natural ability to rewire itself and restore communication with the muscles through neuroplasticity. This mechanism helps strengthen existing neural connections and create new ones. As neural connections are restored, the brain will be able to send nerve signals to the affected muscles, improving mobility and overall function.
Neuroplasticity is best activated through high repetition of rehabilitation exercises. Therefore, to treat foot drop after TBI, consistent practice of foot drop exercises is a must. The more a movement is practiced, the more the brain will reinforce and strengthen the neural connections for that function.
Although foot drop is usually a direct result of a disruption in the brain’s signals to the appropriate muscles, it can also be caused by muscle weakness. Because the cause of foot drop may vary, it’s important to consult with your doctor and obtain an accurate diagnosis.
Understanding the cause of foot drop after TBI is essential to receive the appropriate treatment and maximize the chances of recovery.
Signs of Foot Drop After TBI
One of the most common signs of foot drop after a brain injury is weakness in the foot. However, there are other symptoms your doctor or therapist may look for to make an accurate diagnosis.
Signs of foot drop after TBI can include:
- Curled toes toward the balls of the feet
- Persistent corns on the base of the foot
- Changes in your gait (manner of walking)
- Frequent stumbling and/or falls
It’s important to consult with your doctor if you are experiencing any new or recurring symptoms. They will be able to determine the cause of foot drop and administer the appropriate treatment.
How to Use Ankle Foot Orthotics for Foot Drop After TBI
Because foot drop makes it difficult to move and walk, therapists often recommend using an ankle foot orthotic, or AFO brace. AFOs provide support for the foot and ankle to prevent the toes from dragging on the floor. This helps lower the chances of falling when walking or climbing stairs, reducing the risk of further injury.
While AFOs are helpful, they do not offer a permanent solution for foot drop after TBI. AFOs are considered compensatory tactics, which help compensate for any lost function. Using compensatory tactics is beneficial, especially to protect your safety.
However, when individuals rely on compensatory tactics like AFOs, it can increase the risk of learned non-use, which refers to the suppression of affected body parts. When the affected foot is neglected, it does not encourage movement to return and may further increase reliance on the AFO.
The best way to prevent this from happening is to take breaks from using the AFO and practice foot drop exercises. This will help stimulate the brain and activate neuroplasticity. Additionally, a therapist can provide guidance on which AFO brace is the most suitable for you.
Treatments for Foot Drop After TBI
Along with compensatory tactics, it’s important to find treatments that address the root cause of foot drop after TBI. Although treatments may vary for every survivor, they will most likely include a combination of different options. While we’ve narrowed down the most common treatments for foot drop, it’s important to consult with your doctor first to find safe and effective treatments for your condition.
Treatments for foot drop after TBI may include:
1. Foot Drop Exercises
Since foot drop is often caused by a disruption in communication between your brain and foot muscles, the best way to treat it is to rewire the brain to control dorsiflexion once again. To achieve this, neuroplasticity must be activated through high repetition of rehab exercises.
Foot drop exercises help activate neuroplasticity and restore the connection between your brain and muscles, eventually improving dorsiflexion. Even minimal movement is beneficial and can help stimulate neuroplasticity.
Here are some foot drop exercises for brain injury you can try:
- Ankle eversion: Place your affected foot flat on the ground. Then, lift the outer edge of your foot until your foot is bending inwards. Then, relax back down. Focus on initiating the movement from your ankle only, do not move your leg. Repeat 10 times.
- Negative toe raises: Start by pointing your foot up toward your body as high as you can. Then, instead of quickly letting it drop, slowly lower your foot back down to a neutral position. Repeat 10 times.
- Ankle adduction/abduction: For this exercise, cross your affected leg over the other. Then, using your non-affected hand, move the front part of your foot side to side. Likewise, focus on initiating movement from your ankle. Repeat 10 times.
These are just a few foot drop exercises that can help improve mobility in your foot. But what if your foot drop is extremely severe that you cannot move your foot at all? Survivors with limited to no mobility in their feet can practice passive exercise , another great treatment for foot drop after TBI.
2. Passive Exercise
With passive exercises, survivors can improve foot drop by supporting their foot through correct movement patterns. This can be done by using your hands to move your affected foot through each foot drop exercise. Even passively moving your foot in the correct way can activate neuroplasticity, which will help improve dorsiflexion.
A trained caregiver or therapist can also assist you in practicing passive movements. If you do have some mobility, you can try performing these exercises on your own. Your therapist can provide you with specific exercises that are safe and suitable for you.
Some passive rehab exercises for foot drop include:
- Passive ankle dorsiflexion: Sit in a comfortable position and cross one leg over your other. Then, use your non-affected hand to move your foot up towards your knee and back down. Repeat 10 times, then switch to your other foot.
- Assisted toe raises: If you can only move one foot, this exercise can help you strengthen your other ankle. First, place your non-affected foot underneath your affected one. Then, use your stronger foot to lift your weaker foot. Make sure to always keep your heel on the ground. Then, slowly lower the foot back down. Repeat 10 times.
In addition to stimulating neuroplasticity, passive exercises can also help improve blood flow, lower the risk of contractures, and the chances of developing learned non-use.
3. Functional Electrical Stimulation
While rehab exercises are the best way to promote neuroplasticity and improve foot drop after TBI, some survivors may benefit from additional treatments, such as functional electrical stimulation (FES).
FES involves sending small electrical impulses into the affected muscles of the foot to create a contraction. Reactivating these muscles encourages dorsiflexion and engages neuroplasticity. Ideally, FES should be used in conjunction with rehab exercises, like walking or foot drop exercises, to maximize your chances of recovery.
4. Medication
Prescribed medication can also help treat the symptoms of foot drop and promote the healing of damaged nerves. This can help speed up the process of regaining dorsiflexion. For example, erythropoietin is a hormone naturally produced by the body. This hormone is extremely beneficial because it has anti-inflammatory properties, and it also helps regulate the regrowth of nerves.
Because of its helpful properties, many doctors will prescribe this hormone, along with other similar medications, to help manage foot drop after TBI and promote recovery. However, medication should only be used as added assistance and it should not replace the high repetition of rehab exercises.
Additionally, some medications can have unwanted side effects or interfere with your recovery. Ask your doctor about potential medications for foot drop that are safe for your condition.
5. Surgery
Lastly, severe cases of foot drop may require surgical interventions. Different surgical treatments, such as nerve transfers and decompressive surgery, can help improve dorsiflexion.
Nerve transfers involve taking “donor nerves” from other parts of the body and using them to connect the ends of the divided or damaged nerves. Decompressive surgery is a procedure that helps relieve pressure on the nerves, which can also help improve dorsiflexion. Because surgical interventions are highly invasive, they should only be used when all other treatment options have been exhausted. Talk to your doctor about which type of surgery, if any, is appropriate for you after you’ve exhausted all other options.
Recovering from Foot Drop After TBI
Foot drop after TBI can make it difficult to walk and safely navigate daily activities. The inability to lift the front portion of the foot (dorsiflexion) is caused by the disruption of nerve signals between the brain and muscles.
The best way to improve dorsiflexion and reduce foot drop is to activate neuroplasticity and restore neural connections. This can be achieved by the massed practice of rehab exercises, both active and passive. Still, many survivors will require a combination of treatment including an AFO brace, medication, and a variety of exercises. Therefore, it’s important to consult with your doctor to obtain an accurate diagnosis and rehabilitation plan.
We hope this article helped you understand how a TBI can cause foot drop and how to overcome it.
The post Foot Drop After TBI: Understanding the Causes, Signs, & Treatment Options appeared first on Flint Rehab.



