A lacunar stroke occurs within the deep parts of the brain, such as the thalamus, basal ganglia, or pons. It is a type of ischemic stroke, which occurs when an artery that supplies blood within the brain becomes blocked by a blood clot.
While there are many possible causes, most survivors of lacunar stroke had a preexisting condition that put them at risk. One of the most common risk factors for a lacunar stroke is high blood pressure.
Knowing the causes, symptoms, and potential treatment of a lacunar stroke, or lacunar infarct, can help you and your loved ones be prepared. This article will discuss the signs and symptoms of a lacunar infarct, as well as the rehabilitation process. Before exploring the best ways to promote recovery after a lacunar stroke, it helps to understand what it is and how it can occur.
What Is a Lacunar Stroke?
A lacunar stroke occurs when there is a blockage in an artery that supplies blood to the deep parts of the brain, which can include the thalamus, basal ganglia, and pons.
According to the NIH, lacunar strokes make up one fifth of all ischemic strokes. Most ischemic strokes occur on the surface or cortex of the brain due to blockages in the large arteries. The arteries that lie deep within the brain (or underneath the cortex), are small and vulnerable, making them more susceptible to blood clots.
What Causes a Lacunar Stroke?
Ischemic strokes occur from occlusion, or blockage, of blood supply to a specific part of the brain. This leads to tissue damage and hypoxia when areas of the brain are deprived of oxygen-rich blood.
Occlusion of vascular supply can occur when several medical conditions that narrow the arteries are present. These conditions can increase the risk of a blood clot getting stuck in the arteries.
Some of the most common underlying causes of a lacunar stroke occlusion include:
- Atherosclerosis: a condition in which fatty deposits (plaques) build up in the vessels. When atherosclerosis is present, a clot can also form inside one of the small arteries, interrupting blood flow.
- Lipohyalinosis: a thickening of the blood vessels deep within the brain, making them more susceptible to blockages. This creates less space in your arteries for proper blood flow, making them more prone to blockages.
- Microatheromas: an abnormal mass of fatty or lipid material, which can increase plaque buildup within the innermost layer of an artery.
- Hypertension (High Blood Pressure): can create a bounding pulse, or a strong throbbing felt over the arteries. This condition can cause the arteries to narrow, making it easier for blood clots to form and block blood flow.
- Diabetes Mellitus: a disorder in which the body cannot produce or respond normally to insulin, which causes glucose (sugar levels) to be abnormally high. Unprocessed glucose can then build up in the bloodstream, damaging the blood vessels.
In some cases of a lacunar stroke, small embolic fragments from a cardiac source or large vessel disease can also cause arterial occlusion. For example, a blood clot can form elsewhere in the body and travel to the brain where it may become stuck in one of the small arteries deep within the brain (called an embolic stroke).
The Circle of Willis
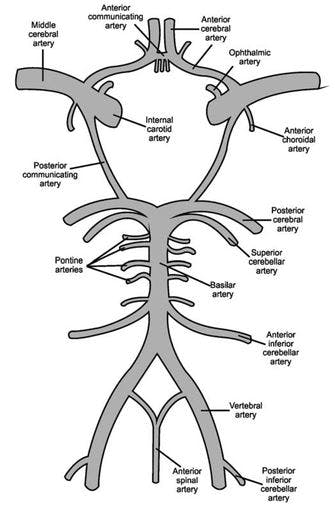
Lacunar infarctions are also caused by occlusion of the small deep penetrating branches of the cerebral vessels in the Circle of Willis. The Circle of Willis consists of several major arteries that encircle the middle of the brain. A lacunar stroke can occur when one of the perforating branches of the Circle of Willis, an important part of blood supply within the brain, becomes blocked.
The Circle of Willis also serves as a safety mechanism for blood flow. When a blockage or narrowing in the arteries slows or prevents blood flow in a connected artery, the change in pressure can cause blood to flow forward or backward in the Circle of Willis to compensate. This safety mechanism helps blood flow from one side of the brain to the other when the arteries on one side have reduced blood flow.
In an emergency situation like a stroke, this mechanism may help reduce the damage or aftermath of the event. The Circle of Willis itself does not actively carry out the function, rather the natural shape of the circle and natural pressure within the area allow for bidirectional blood flow when needed.
Risk Factors of a Lacunar Stroke
Lacunar strokes make up about one fifth of ischemic strokes. It’s important to understand the risk factors to help prevent this type of stroke. These risk factors closely resemble the general leading causes of stroke.
Common risk factors that can eventually lead to a lacunar stroke include:
- Hypertension (high blood pressure)
- Diabetes mellitus
- Hyperlipidemia
- High LDL cholesterol
- History of stroke
- Carotid artery atherosclerosis
- Peripheral artery disease
- Hyperhomocysteinemia
- Other cardiovascular diseases
- Genetic conditions
Smoking, obesity, and low physical activity are also risk factors for other types of ischemic strokes. However, two of the most common risk factors seen in lacunar and non-lacunar ischemic strokes are hypertension and diabetes.
Signs and Symptoms of a Lacunar Infarction
Brain cells support different functions throughout the body. When a lacunar stroke occurs and brain cells are deprived of oxygen, they can die within minutes, interfering with functions such as speech and movement.
Learning how to recognize the signs of a stroke is important to be able to help someone receive timely emergency care.
Signs of a lacunar stroke can include:
- Weakness or drooping on one side of the body
- Ataxia (impaired coordination on one side of the body)
- Changes in sensations such as temperature, touch, or taste
- Facial weakness (especially in the tongue or larynx)
- Difficulty with fine motor skills
- Difficulty speaking or understanding language
- Slurred speech
- Inability to raise one arm
- Numbness
- Confusion
- Memory problems
- Headache
However, because lacunar infarcts are small, individuals may not develop noticeable symptoms. Sometimes they can even show up on brain scans before people are aware of them.
How Is a Lacunar Infarct Diagnosed?
To diagnose a lacunar stroke, doctors will first evaluate symptoms in the emergency room. They will most likely order a CT Scan not to identify the stroke but to rule out other conditions with similar symptoms. Then, your doctor may order a CT Angiogram, where they administer dye into your blood vessels to help them show up on the scan.
With these tools, doctors may see blockages in the vessels related to atherosclerosis. They may also order an MRI (Magnetic Resonance Imaging), which is one of the most accurate imaging tests for a lacunar stroke diagnosis. Clinical presentation and neuroimaging are key components of a lacunar stroke diagnosis because lesions tend to be small and lack edema or swelling.
Doctors may also look for lacunar syndromes, which are a group of symptoms that occur in a fluctuating manner, to help differentiate a lacunar stroke from other types of strokes.
There are over 20 lacunar syndromes that have been described, but 5 of the most common include:
- Pure motor hemiparesis: weakness in the face, arms, and legs with no other deficits and usually an internal capsule lesion.
- Ataxic hemiparesis: weakness and ataxia (impaired balance or coordination) on the same side. Lesions can vary from the posterior internal capsule, midbrain, or pons.
- Dysarthria and clumsy hand syndrome: tongue and face weakness with clumsy hands on the same side.
- Pure sensory stroke: loss of sensation, usually an indication that the lacunar stroke impacted the thalamus
- Sensorimotor stroke: combination of motor and sensory strokes
While lacunar syndromes can help identify the type of disease, they may not show the exact location of the lesion. As previously mentioned, lacunar strokes arise from occlusion of the small branches of both the anterior and posterior vessels, most commonly the Circle of Willis.
Treatment for a Lacunar Stroke
Initial treatment of a lacunar stroke follows similar steps for all ischemic strokes. Depending on the stroke symptoms and duration such as 4 and half hours or less, doctors may perform thrombolysis. This is a procedure using either medication or a mechanical device to break up blood clots that disrupt blood flow in the arteries and veins.
Depending on the severity and if the symptoms have lasted longer than 4 and a half hours (but less than 24 hours), doctors may perform a thrombectomy. This is a more invasive treatment in which the blood clots are surgically removed.
Emergency treatment is crucial for all types of stroke including lacunar. Therefore, it’s imperative to seek immediate medical care if you or a loved one experience any of the signs or symptoms.
Following initial treatment, doctors will most likely prescribe blood-thinning drugs to prevent more blood clots from developing. Your doctor may also prescribe medication to help manage cholesterol, blood pressure, and sugar levels to reduce the risk of another stroke.
Long-Term Effects of a Lacunar Stroke
Symptoms of a lacunar stroke may vary depending on the areas of the brain affected such as the basal ganglia or thalamus.
Survivors can recover from a lacunar stroke, sometimes with a better outlook than other types of strokes. However, research has shown that a lacunar infarct can increase the risk of further strokes as well as cardiovascular diseases, and dementia, so it’s important to prioritize stroke prevention (which we discuss later) after a lacunar stroke.
Recovery from a lacunar stroke involves identifying the secondary effects and creating a rehabilitation plan to address those effects. Some of the long-term effects of a lacunar infarct include:
- Paralysis
- Numbness
- Loss of muscle control on one side of the body
- A tingling sensation in the affected limb(s)
During stroke recovery, survivors may also experience difficulty with short-term memory, thinking, reasoning, and controlling emotions. Some survivors may also struggle with depression after a lacunar stroke. Understanding the potential long-term effects of a lacunar infarct is important to ensure you and your loved one get the proper care.
Rehabilitation After a Lacunar Stroke
Rehabilitation after a lacunar stroke varies for every survivor depending on the severity and location of the stroke. For example, a lacunar stroke that impacts the thalamus can cause changes in sensation because the thalamus relays over 98% of sensory input. If a lacunar stroke impacts the basal ganglia, which contributes to voluntary muscle control, it can result in changes in motor function.
Fortunately, many of the secondary effects caused by a lacunar stroke can be restored through rehabilitation and the promotion of neuroplasticity, the brain’s ability to rewire itself. When neural pathways in the brain become damaged after stroke, neuroplasticity helps the brain create and strengthen new ones.
Neuroplasticity is best activated through high repetition of exercises, or massed practice, which is the focus of the rehabilitation process. Therefore, it’s essential to work with your doctor or therapist to find the best therapy exercises for your ability level.
Generally, after a lacunar stroke, therapy will focus on restoring function, improving your ability level, and stimulating neuroplasticity. Treatment may include a variety of different therapies, such as:
Occupational Therapy

Occupational therapy helps you maximize independence with the activities of daily living such as eating and bathing. An occupational therapist can provide you with various treatment ideas after a lacunar stroke which can include task-specific training exercises.
They may also recommend using occupational therapy tools to help you achieve your goals as you rebuild strength. For example, adaptive utensils can make eating easier after a lacunar stroke while still promoting the use of fine motor skills.
Physical Therapy
Physical therapy, along with occupational therapy, is essential to help improve motor-related secondary effects after a lacunar stroke. For example, survivors who experience hemiparesis, or weakness on one side of the body, can benefit from physical therapy exercises that help stimulate neuroplasticity and retrain the affected muscles.
Your physical therapist can provide you with a variety of stroke recovery exercises to help retrain the affected limbs. The more you practice moving your affected side, the higher the chances of restoring function.
Speech-Language Therapy

Many survivors may experience dysarthria (weakness in the muscles that cause slow or slurred speech) after a lacunar stroke. Fortunately, speech-language therapy can help survivors improve their speech by retraining the muscles that control the mouth. Speech-Language Pathologists (SLP) are experts in providing speech therapy exercises that target the muscles used for speech, which can also help improve swallowing difficulties.
To stay engaged in therapy between visits, you can either follow along to a sheet of exercises or use motivating speech therapy apps like the CT Speech and Cognitive Therapy App. Created by two SLPs, the CT App provides access to over 10,000+ speech therapy exercises that you can do anytime from the comfort of your own home.
Sensory Retraining
After a lacunar stroke, survivors may also experience loss of sensation. This can occur when the somatosensory cortex does not receive or process the information necessary. Fortunately, sensory retraining (sensory reeducation) can help promote the return of sensation after a lacunar infarct.
Sensory retraining exercises involve safely exposing yourself to various sensory stimuli that help activate neuroplasticity in the brain. For example, if you struggle with numbness after a stroke, you can place items with different textures in a bowl of uncooked rice and practice fishing for them without looking. Speak with your occupational therapist to learn more about sensory retraining.
Home Therapy

After inpatient rehabilitation, many survivors are discharged home to continue recovery, while visiting an outpatient therapist once a week. However, it’s important to continue to engage in therapy daily to promote neuroplasticity and maximize recovery after a lacunar stroke.
To keep yourself motivated to exercise at home, you can try gamified neurorehabilitation devices such as FitMi and MusicGlove. FitMi is an interactive neurorehab device designed to improve mobility after a stroke by motivating you to accomplish high repetition of full-body rehabilitation exercises. It’s versatile and allows you to target different muscle groups based on your ability level and unlocks harder exercises as you improve.
MusicGlove is another popular at-home neurorehabilitation device. It’s a music-based hand therapy device that has been clinically proven to help survivors improve hand function in just 2 weeks. Many survivors become immersed in the experience and forget they are doing physical therapy.
How to Help Prevent a Stroke
A lacunar stroke can be life-threatening if left untreated. Therefore immediate medical care is important. While there are some risk factors that cannot be controlled, such as age or genetics, there are other risk factors that can be managed through lifestyle modification.
Developing healthier habits such as maintaining a balanced diet, exercising for about 30 minutes daily, and avoiding smoking altogether can also help decrease the chance of stroke. Excess sodium can increase blood pressure, and excess sugar can exacerbate diabetes. Therefore, it’s important to cut down on sugar, salt, and fatty foods, especially if you have any preexisting medical conditions.
Along with dietary changes, prevention can include prescribed medication to manage risk factors like hypertension or antithrombotic medication like aspirin and ticlopidine (blood thinner that keeps blood clots from forming in the vessels).
While antiplatelet agents help lower the risk of recurrence lacunar strokes, blood thinners like aspirin may be dangerous if administered without a doctor’s approval. Therefore, consult with your doctor to learn more about preventative care suitable for your condition.
Understanding a Lacunar Stroke
A lacunar stroke is a type of ischemic stroke that occurs when the small arteries deep within the brain become blocked. Risk factors like high blood pressure, diabetes mellitus, and smoking can increase the risk of lacunar stroke.
Immediate medical care is crucial to restore the flow of blood within the brain. Following initial treatment is the rehabilitation process which can include a variety of different therapies. The goal of rehabilitation is to activate neuroplasticity, restore as much function as possible, and maximize independence.
We hope this article helped you understand what a lunar stroke is and what signs and symptoms to look out for. While a lacunar infarct may be complex, there are many ways to promote recovery.
The post Lacunar Stroke: Understanding the Causes, Symptoms, and Treatment appeared first on Flint Rehab.



