A C3 spinal cord injury is a type of cervical spinal cord injury. Survivors of a C3 spinal cord injury can experience movement and sensation changes from the neck down. Depending on the severity of the injury, some survivors lose feeling and become completely paralyzed in the arms, legs, and trunk, while others may retain some sensation and/or movement.
Fortunately, by participating in rehabilitative therapies and effectively managing secondary complications, individuals can learn to become as functional as possible and maybe even recover sensory and motor functions.
To help you understand what to expect after a C3 SCI, this article will discuss potential effects and how to manage them. Use the links below to jump directly to any section.
What is a C3 Spinal Cord Injury?
The spinal cord is a bundle of nerves that act as a connection between the brain and the rest of the body. Thirty-one pairs of nerves branch out from the spinal cord, transmitting motor and sensory messages to and from the body. A C3 spinal cord injury occurs when damage to the spinal cord damage limits the ability for information to be transmitted past the 3rd set of cervical nerves. When the spinal cord becomes injured, sensory and motor messages are unable to be transmitted properly, resulting in affected functions below the level of injury.
The uppermost area of the spinal cord, located within the neck, is referred to as the cervical region. The cervical spinal nerves transmit messages between the brain and body regarding movement and sensation of the head, neck and arms. In survivors of a C3 SCI, the spinal cord is damaged directly below the third pair of cervical spinal nerves. This means that individuals with C3 injuries only have 3 pairs of spinal nerves that are fully intact. Therefore, depending on the completeness of the injury, all sensory and motor functions related to nerves below the C3 level may be lost.
C3 Spinal Cord Injury Diagnosis and Classification
Doctors may use various tools to diagnose a C3 spinal cord injury. Along with a CT scan and/or MRI, medical professionals typically use physical tests, including an assessment called the ASIA exam. This assessment involves testing sensory and motor functions specific to each level of the spinal cord in order to determine the severity and level of injury.
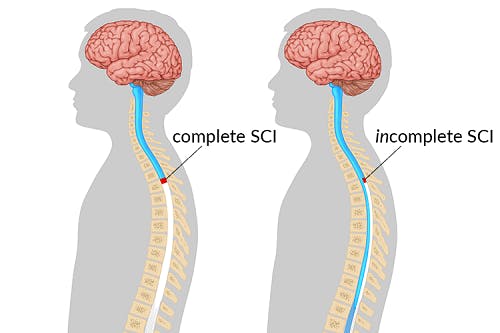
The severity of a spinal cord injury significantly affects one’s functional outcomes and recovery outlook. A spinal cord injury can be classified as complete or incomplete.
Complete spinal cord injuries are the most severe, resulting in a loss of all sensory and motor functions below the level of injury. In survivors with complete spinal cord injuries, the spinal cord has been completely severed, leaving no spared neural pathways. Since there is no way for messages to be transmitted through the damaged area, no motor control or sensation will exist below the level of injury.
In contrast, an incomplete spinal cord injury refers to partial spinal cord damage. Some neural pathways are spared and consequently, some motor and/or sensory functions below the level of injury may be unaffected. Incomplete spinal cord injuries may also vary in severity, depending on how many neural pathways are spared.
When individuals sustain a C3 spinal cord injury, the first three pairs of spinal nerves (C1, C2, and C3) are left intact. These nerves are able to transmit sensory and motor information to and from the brain, meaning that sensation and movement functions associated with these nerves remains intact.
The C1 and C2 segments of the spinal cord generally control the muscles that allow you to nod your head up and down as well as sensation at the upper neck and the back portion of the head. The C3 spinal nerves are responsible for sensation in the neck area as well as neck side flexion, which is the ability to tilt your neck to each side.
As a result, individuals with C3 spinal cord injuries should be able to feel and move their head and neck normally. Depending on the severity of the injury, functions below the neck may or may not be affected. Functional outcomes and the onset of secondary complications can vary significantly.
Potential Effects of C3 Spinal Cord Injury
Every C3 spinal cord injury is different. Having an idea of what to expect can help individuals adjust to life after a C3 SCI. Below are 7 of the most common effects that survivors of a C3 spinal cord injury may experience.
1. Breathing Difficulties

A C3 spinal cord injury can affect the muscles involved with breathing which, without immediate medical attention, can be fatal. This is because the primary muscle involved in respiration, called the diaphragm, is controlled by the C3-C5 spinal nerves.
Individuals with C3 spinal cord injuries often require ventilator assistance to restore breathing, at least initially. Depending on the severity of the injury and the effectiveness of rehabilitative interventions, it is possible for individuals to strengthen breathing functions and gradually wean off ventilator dependence.
2. Paralysis from the Neck Down
A C3 spinal cord injury results in quadriplegia, which refers to paralysis of the arms, trunk, and legs.
Depending on the severity of your spinal cord injury, some survivors may be able to move and/or feel sensation below your level of injury.
However, in the case of a complete C3 SCI, individuals experience paralysis of the entire body below the neck and require full-time caregiver assistance.
3. Changes in Body Composition
Because spinal cord injuries at the C3 level can significantly affect most body movements, individuals often experience physical changes to the body as a result of limited active movement
Consequences of reduced physical activity include:
- Reduced bone density
- Muscle atrophy
- Poor circulation
- Lowered resting metabolic rate
Likewise, individuals may initially lose a substantial amount of weight due to reduced bone density and muscle mass. However, they may also gain weight if they continue to consume the same amount of food as they did when they were more physically active.
4. Bowel and Bladder Dysfunction
If messages from the bowel and bladder cannot pass through the damage in the spinal cord to reach the brain, then individuals with C3 spinal cord injuries may experience changes to their bowel and bladder functions. As a result, they will not be able to sense when their bladder or bowels are full and are susceptible to leaking and accidents. Furthermore, if the brain is unable to send messages to the bowel and bladder muscles to contract or relax, eliminating waste at appropriate times becomes challenging.
Complications of bladder and bowel dysfunction include urinary retention, kidney damage, infection, and constipation.
To prevent bowel and bladder-related accidents from occurring, it’s essential for individuals with C3 SCIs to follow a bowel and bladder program.
5. Pressure Sores
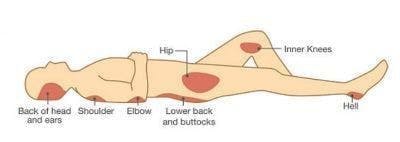
Since movement of the arms, legs, and trunk is often limited in those with a C3 SCI, individuals are more likely to remain in one position for an extended period. If individuals lose sensation after a C3 spinal cord injury, they likely won’t feel uncomfortable remaining in the same position for a prolonged time. However, failure to frequently change positions places excess pressure on certain parts of the skin, which can cut off blood flow and cause the skin to break down. Areas of skin breakdown due to prolonged pressure on certain areas of the body are known as pressure sores.
Pressure sores most commonly develop in bony areas like the hip bones, heels, knees, tailbone, and elbows.
To prevent pressure sores from developing, it is essential to change positions every two hours when lying in bed or every 30 minutes when sitting in a wheelchair. Additionally, inspecting the skin daily for any signs of redness or irritation can help identify and treat pressure sores early before they become problematic.
6. Autonomic Dysreflexia
The autonomic nervous system regulates involuntary body functions like body temperature, blood pressure, and heart rate. After a C3 spinal cord injury, individuals may experience autonomic dysreflexia, which occurs when these functions become hyperactive due to the disrupted transmission of messages between the brain and body.
Generally, any stimulation (wearing tight clothes, extreme temperatures, pressure sores, etc.) below the level of injury can trigger autonomic dysreflexia. As a result, individuals may experience a spike in blood pressure, feelings of panic, and flushed skin.
Because signals from the brain may not be able to reach areas below the level of injury, individuals may experience contrasting symptoms above and below their level of injury.
Generally, autonomic dysreflexia can be resolved by identifying what is triggering the episode and removing it. It’s essential for individuals with C3 spinal cord injuries and their caregivers to be alert and mindful of their surroundings. If symptoms persist, seek immediate medical attention.
7. Spasticity
Following a C3 spinal cord injury, individuals may experience spasticity. Spasticity describes involuntary muscle contractions that can worsen with movement.
Because messages between the brain and areas below the level of injury are disrupted by SCI, spastic muscles are unable to receive signals from the brain to relax and therefore remain tightened. This can cause stiff movements, muscle spasms, and chronic pain.
While the potential effects of a C3 spinal cord injury are significant, there are many ways to effectively manage these effects and pursue recovery.
C3 Spinal Cord Injury Recovery
Every C3 spinal cord injury is unique, and every journey to recovery looks different. Depending on your personal goals and circumstances, treatment may focus on rehabilitative therapy, compensatory tactics, or a combination of both. The goal of rehabilitative therapy is to regain lost functions. On the other hand, a focus on compensatory tactics allows individuals to optimize their independence by finding ways to work around lost functions.
One of the primary factors affecting recovery after a C3 SCI is the severity of the injury. Those with incomplete spinal cord injuries have spared neural pathways, meaning that there are still some connections remaining between the brain and the rest of the body. These spared connections are able to take advantage of the central nervous system’s ability to rewire itself through a process called neuroplasticity. This allows the spinal cord to adapt and reorganize itself so that functions lost or weakened by SCI can be relearned. Neuroplasticity is activated by repetitive practice of exercises and activities involving affected functions, making rehabilitation essential for recovering sensory and motor functions. The less severe a spinal cord injury is, the more spared neural pathways exist, and the better the recovery outlook.
Conversely, individuals who have sustained a complete injury often focus on compensatory tactics. Although there are some new treatment options currently being studied for those with complete spinal cord injuries, functions often cannot be recovered due to the lack of spared neural connections. Compensatory tactics can allow those with complete SCIs to reframe their definition of recovery, putting a focus on optimizing independence and quality of life, rather than on regaining lost functions.
Therefore, a personalized rehabilitation plan that addresses your specific needs is essential. Rehabilitation for C3 spinal cord injuries can consist of:
- Physical therapy. A physical therapist can assess your functional abilities and guide you through targeted exercises that can help you improve your mobility and strength. They may also use specialized techniques, such as electrical stimulation. Consistently practicing physical therapy exercises, even if only passively, will help promote neuroadaptive changes in the spinal cord. Physical therapists also can provide home exercise programs, which are essential for promoting neuroplasticity for a greater recovery.
- Occupational therapy. Occupational therapists use a combination of rehabilitative therapy and compensatory tactics in order to promote independence in the activities of daily living (personal care tasks such as dressing and bathing) and other daily activities. They may recommend adaptive equipment or assistive technology, such as a voice activated or eye gaze controlled computer or wheelchair. Occupational therapists can also provide caregiver training to facilitate safety in the survivor’s day to day life.
- Speech therapy. Individuals with weakened respiratory functions after a C3 SCI should work with a speech therapist for a voice assessment and related impairments. If needed, speech therapists can recommend alternative forms of communication to allow those with a C3 SCI to communicate effectively.
- Psychotherapy. Adjusting to life after a C3 SCI can be difficult and take a toll on your mental health. Working with a psychotherapist can help you learn effective ways to cope.
- Medications. Medications may be prescribed to help manage secondary complications like pain, spasticity, and depression.
- Orthotics. Orthotic devices like braces and splints will help promote correct musculoskeletal alignment.
- Bowel and bladder programs. Following a bowel and bladder program will help prevent bowel and bladder-related accidents. This can involve following a schedule, catheterization, and using suppositories.
- Dietary changes. Modifying your diet can help prevent excess weight gain, promote bowel and bladder movements, and improve energy levels to participate in rehabilitative therapies.
- New treatments. Researchers are constantly studying new techniques for improving SCI recovery. Studies on epidural stimulation and stem cell therapy are currently underway for those with complete cervical SCIs. This can provide those with a complete C3 spinal cord injury with hope for a more functional recovery in the future.
While adjusting to a C3 spinal cord injury can be challenging, many C3 SCI survivors are able to lead fulfilling lives with appropriate management techniques. Those with complete spinal cord injuries are often able to use alternative controls to operate a power wheelchair independently. Positioning devices to promote musculoskeletal alignment may also be custom-made to fit the individual’s needs, allowing them to sit up more comfortably. Controls activated though eye-gaze, head movements, or voice commands can also make technology accessible, allowing individuals to communicate through calling or texting, play video games, and surf the internet. Having full control of the head and neck can increase the ability to engage in different hobbies, such as painting using the mouth to hold the paintbrush. Although those with a complete C3 spinal cord injury will require full-time caregiver assistance, there are still many creative ways to engage in meaningful life activities.
Understanding C3 Spinal Cord Injury
A C3 spinal cord injury can affect movement and sensation below the neck. However, depending on the severity of their injury, individuals may be able to move or feel areas below the level of injury.
By participating in rehabilitative therapies and effectively managing secondary complications, individuals can become as functional as possible and improve their quality of life.
Hopefully, this article helped you better understand the effects of a C3 spinal cord injury.
The post C3 Spinal Cord Injury: What to Expect and How to Recover appeared first on Flint Rehab.



